I am one of the ~3M people in the USA that experiences gastroesophageal reflux disease (GERD). I can eat throughout the day with only minor symptoms, but an hour after my evening meal I get those familiar, and very uncomfortable symptoms of a burning in my chest, which sometimes includes burning in my throat, especially when I burp. Changes to my lifestyle and the GERD diet is supposed to help, so what is the GERD diet and exactly how does it help?
—**—
My GERD Story
For several decades I was on an anti-inflamatory medicine that managed the pain and inflammation of osteoarthritis, which I have at various critical parts of my anatomy. A side effect of that medicine was I developed GERD and wound up having to also take proton pump inhibitors (PPIs). After decades of taking these drugs, concerns were raised in the literature about long term adverse effects of both of the drugs on people’s overall health. So I moved off them about 5 years ago due to losing a lot of weight (80#) and moving onto a different arthritis medicine that does not cause heartburn.
However, about 1 year ago things changed, and it was not the drugs I was taking. I started to gain some of the weight back, ~45#, and started experiencing some food allergies. All of a sudden I am now experiencing the same GERD-related symptoms as before. So I thought it best to start finding out more about my allergies and the GERD diet.

GERD Research
What is GERD?
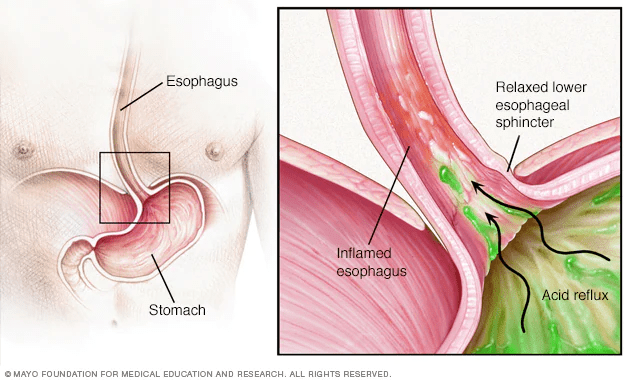
Mayo Clinic describes GERD as a digestive disorder or disease, where stomach acid (or bile) irritates the food pipe lining.
- HopkinsMedicine: the esophageal sphincter (a muscular tube that lets food pass into the stomach and then cinches shut to block it from coming back up) protects the esophagus from stomach acid. However, if the sphincter relaxes, food can push upward through the loosened opening and cause acid reflux.
While this can occasionally happen to all of us, having incidents consistently, more than twice a week, may indicate GERD. Usually this is a self-identified illness that people tend to self medicate with OTC drugs like Prilosec and Tums. When this does not work, they then tend to eventually go to the doctor for review and assistance. Frankly, if you experience these symptoms (consistently) for more than 2x a week please consult with your doctor.
Symptoms of GERD?
- Heart burn
- Mine worsens in the evenings
- Or when I am lying down flat
- Chest pain
- Regurgitating or burping
- Sensation of a lump in the throat
Additionally there are some other symptoms, some of which I have experienced.
- Coughing
- Especially after eating
- Chronic laryngitis
- Disrupted sleep
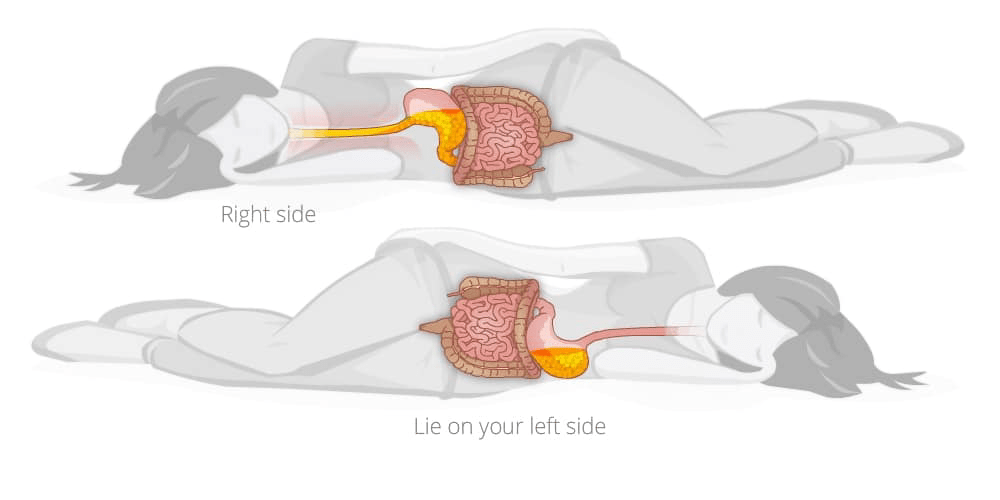
- Worsening burning if lying on right side, better on left side
Conditions Leading to GERD
The western medical field lists many conditions that may lead to GERD, here is just a handful:
- Medication side effect
- Obesity
- Diabetes
- Esophagitis (damage to the esophagus)
- Hiatal hernia (where part of the stomach pushes up through the diaphragm)
- Barrett’s esophagus (damage to the lower part of esophagus)
- Acute bronchitis (inflammation of bronchial tubes lining)
- Metabolic syndrome
- Gastritis (inflamed stomach lining)
- Asthma
- Bulimia
- Stomach ulcer(s)
- Irritable bowel syndrome
- Connective tissue disorders
Lifestyle choices also can lead to or exacerbate GERD.
- Pregnant
- Smoking
- Eating very large meals
- Eating too fast so food is not properly digested
- Eating late at night, close to bed time
- Eating certain foods (fatty or fried for example)
- Drinking alcohol or coffee
- Wearing tight fitting clothes or belts
- Constantly stressed
Medications/Supplements Exacerbate GERD
As in my story, some medications can start or exacerbate GERD. Here is a partial list I gleaned from all the sites I reference in this article.
- Anticholinergics
- Antibiotics
- Calcium channel blockers, statins, ACE inhibitors and nitrates
- Iron supplements
- Narcotics such as codeine, and those containing hydrocodone and acetaminophen
- Oral Bisphosphonates
- Pain relievers (including ibuprofen and aspirin)
- Potassium supplements
- Progesterone
- Quinidine
- Sedatives or tranquilizers
- Theophylline
- Tricyclic antidepressants
When to Seek Medical Advice
WebMD lists several items that require a visit to your medical professional:
- If you have taken OTC meds to treat the symptoms of GERD and it continues
- If having symptoms of a heart attack
- If vomiting blood
- If stools become dark and bloody
Solutions to GERD
According to the International Foundation for Functional Gastrointestinal Disorders (IFFGD), we all have differing triggers. So the first thing I wanted to do was to identify all the relevant lifestyle and diet choices I have made, and identify those that worsen or cause heartburn symptoms. My goal was to reduce my long term use of antacids since that can cause other issues, like B12 deficiency (1).
Lifestyle Changes
In terms of lifestyle choices I listed out what I should be doing and modified my behavior to match the suggestions where I could.
- Eat earlier, so there is 3-4 hours before bedtime
- Eating mindfully, slowly so you thoroughly digest the food
- Keep good posture during and 2 hours after a meal, no reclining or lying down
- Wear loose clothing and avoid belts
- Meditate or exercise to deal with stress
- Change sleeping habits to raise head ~6-8” for gravity to help (2), avoid or limit sleeping on your right side, avoid naps, and make sleeping a routine (3)
- Eat smaller portions at one sitting (4)
- Avoid constipation by upping fiber intake
- Maintain a healthy weight (5)
- Stop smoking, as nicotine loosens the lower esophageal muscle (6)
- Healthline suggests chewing gum after eating, but not spearmint or peppermint
Diet Changes: Avoidance
In terms of food specifically, I am looking at avoiding or limiting certain foods as they are triggers for many people affected by GERD, and can worsen symptoms. If I just cannot avoid these foods, then I try to eat them early in the day so I do not consume them at night.
- High-fat foods (including all fast foods and processed foods)
- Deli meats (bacon, sausage, etc.)
- Cheese
- Spicy foods (chili powder, cayenne, pepper)
- Chocolate
- Peppermint
- Citrus, pineapple
- Tomato and tomato products
- Carbonated or alcohol or caffeine drinks
- Overly salted food
Some references, like MedicalNewsToday, indicate chocolate, mint, carbonated beverages, acidic drinks, caffeine and tomato sauce have little clinical evidence linking these foods to GERD symptoms, but the anecdotal experiences of some people with the condition suggest that these foods may worsen symptoms.
Diet Changes: Consume
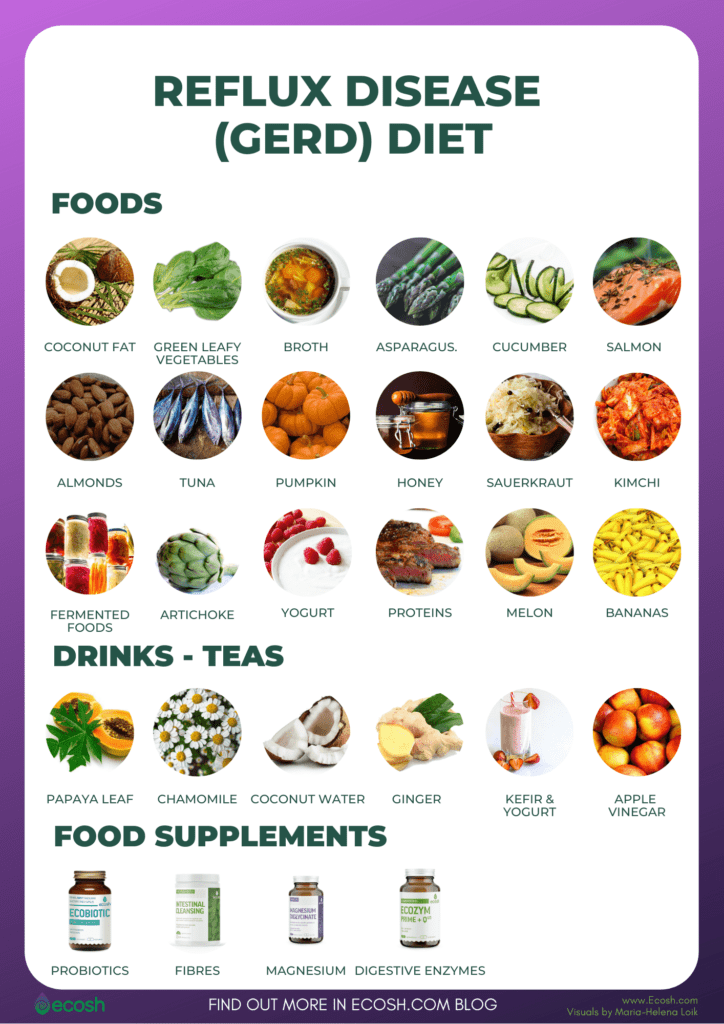
HopkinsMedicine and all the references I have used suggested some foods to eat as a way to assist in the reduction of symptoms.
High fiber consumption is mentioned as a good thing toward easing symptoms. This means adding whole grains, root veggies, and green veggies to ones diet. The reasoning is these high-fiber foods will make me feel fuller, quicker, and are thus to lower the portion sizes I may eat.
Another idea is to eat more alkaline foods to offset the acidity. Although lemons turn alkaline in our bodies they are not on this list. Instead, consume more bananas, melons, cauliflower, fennel, and nuts. While I am not a heavy fennel eater (I do not really like the licorice taste or aroma) I have been increasingly using this veggie as part of a Mediterranean meal.
Another idea is to eat a diet filled with watery foods. Obviously this includes watermelon, cucumber, lettuce, and celery. But also this can include various soups and herbal teas.
MedicalNewsToday suggests consuming fermented food like sauerkraut, kefir, and kombucha.
Eating lean-proteins are mentioned in AboutGERD as something to consider. But also to focus on consuming healthy fats.
- Monounsaturated fats. Examples include oils such as olive, sesame, canola, and sunflower; avocados; peanuts and peanut butter; and many nuts and seeds.
- Polyunsaturated fats. Examples include oils such as safflower, soybean, corn, flaxseed, and walnut; soybeans and tofu; and fatty fish such as salmon and trout.
Home Remedies
This “home remedies“ section is not implying a cure to GERD, nor am I attempting to practice medicine. These comments cannot replace speaking with your doctor, nurse, dietician, or nutritionist about your medical condition. I am just a cook and not a professional medical practitioner.
Last night I drank 8oz of non-fat milk to help ease the immediate pain. Whole milk contains more fat, so non-fat or reduced-fat will help better. This will only be temporary but sometimes is enough. Other people I know also use low-fat yogurt, since that has probiotics.
When I drink my Earl Gray tea each morning, I have been adding juice from 1/2 a lemon and 1T of honey to offset the caffeine drink. Some people say honey-lemon water helps them; the lemon turns alkaline in the body, and honey has anti-inflammation properties. I will have to test, I think I am drinking too much caffeinated tea in one day, as I average 40oz. So this is one of the things I will modify.
Drinking slippery elm tea may help coat the throat and is one way to temporarily ease symptoms (7).
Other people I know swear by drinking apple cider vinegar, which I have not tried. I have one friend in particular, Trader Joe’s Jill who loves vinegar and could drink it straight. Perhaps if I avoid creamy salad dressing and focus on oil + mainly vinegar dressings I can improve the symptoms?
I already know ginger to be a digestive aid used by many across the world. It is alkaline and is suppose to aid in reducing inflammation. So one thing I may try in the future is sipping a ginger tea when I feel the symptoms starting. My only problem is I do not like the overwhelming taste of ginger, my preference is just for a hint in the foods I make. So this one may be a hard option for me.
Non-Western Medicine
Traditional Chinese Medicine, a 2k+ older healing technique suggesting that liver or stomach issues can lead to internal imbalances, that also lead to GERD. These practitioners may explain that daily stress and frustrations, combined with “fiery” foods, can: build up a “stomach fire”, “liver fire”, or a “dampness” in the stomach. Common suggestions for lifestyle and food chances include:
- Incorporating vinegar, kiwis, tomatoes, lemons and limes into your diet can cool the liver and soothe your nerves.
- Consume “cool” foods like celery, cucumber, eggplant, green or mint tea, lotus root, aloe vera, bananas and melons
- Use meditation, yoga, or other movement de-stressers to calm body systems.
- Avoid dampness.
More Study Needed
While I am working on self-treatment at this point, it should be noted that there are lots of questions remaining about GERD. For one, there may be differences among populations. Studies have shown:
- The highest rate of GERD among older, non-Hispanic, married, more educated women who also have Crohn’s disease, endometriosis, and thyroid ailments.
- Highest failure to ease systems rate among PPI users were younger, female, Latino, married, employed, and had irritable bowel syndrome.
- GERD can cause Barrett’s Esophagus (which in turn can lead to esophageal adenocarcinoma) is more prevalent in caucasian males, people older than age 50, smokers, and overweight.
- Over the past decade, science has also shown that long-term use of PPIs to control GERD is problematic with conerns including risk of fractures, pneumonia, Clostridium difficilediarrhea, hypomagnesemia, vitamin B12 deficiency, chronic kidney disease, and dementia.
Clearly, while trying to prevent or lesson the painful symptoms, we need to know more about this ailment and how different populations experience the disease. Further, we need to better understand how to treat by diet and lifestyle changes within various communities. But those of us experiencing these symptoms can take an affirmative hand in our treatment. Starting with changing our lifestyle habits, and modifying our diets.
—Patty
—**—
Hi there! Someonee in my Facebook group shared ths
website with uss sso I camje too give it a look. I’m definitly enjoying the information. I’m book-marking andd will be tweeting this too
my followers! Excellent blog and excellent design andd
style.